Collaborators: Helia Haghoost, Martina Masina and Jennifer Byrne
Skin health professionals can play an important role in providing education about sun protection and the effects of sun exposure on skin health. Skin health professionals may see their clients regularly sometimes over years and are therefore well placed to support with re-enforcing sun-safe behaviours.

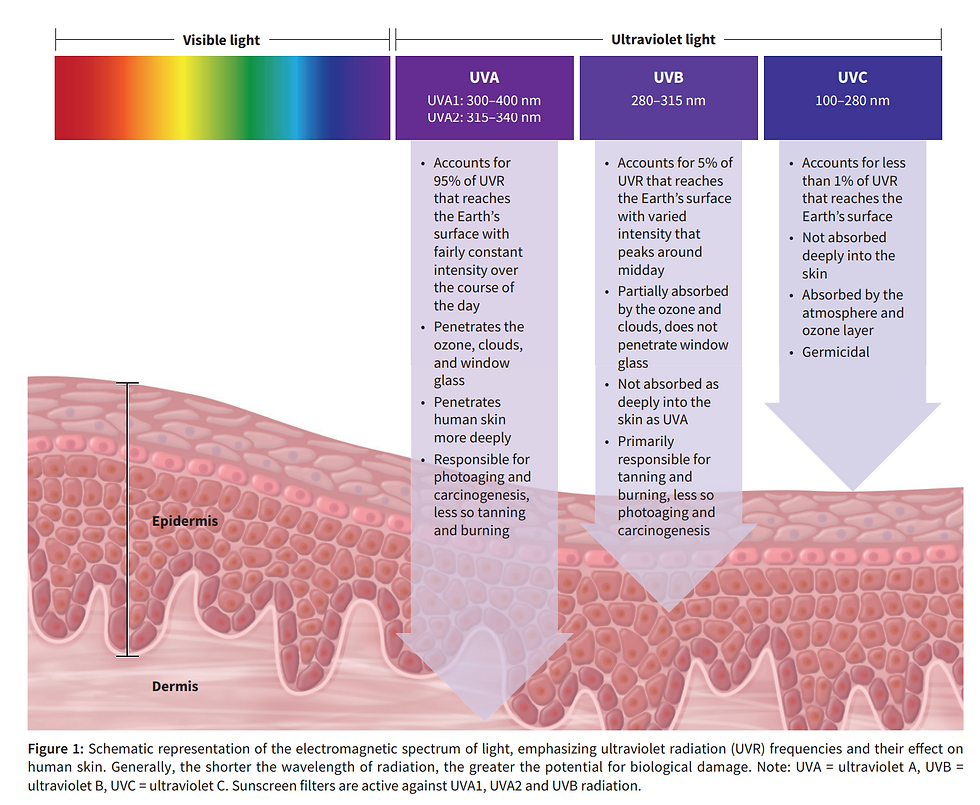
The sun emits Ultraviolet radiation which is the main culprit for skin damage. UV rays are invisible and cover wavelengths shorter than visible light and longer than X-rays and constitute 5% of iridescent sunlight. UV radiation covers the spectrum of wavelengths from 100 to 400 nm.
Ultraviolet radiation leads to the formation of reactive oxygen species (ROS). ROS are responsible for the creation of free radicals which leads to direct damage to cutaneous DNA, lipids, proteins, damage to membranes and it is responsible for photocarcinogenesis. Ultraviolet radiation is subcategorised as UVA, UVB and UVC rays, each with specific characteristics and tissue interaction.
Sander M, Sander M, Burbidge T, Beecker J. The efficacy and safety of sunscreen use for the prevention of skin cancer. CMAJ. 2020 Dec 14;192(50):E1802-E1808. doi: 10.1503/cmaj.201085. PMID: 33318091; PMCID: PMC7759112.
What are UVAs
UVA covers the wavelengths of 320nm to 400nm with consistent year-round intensity. Due to possessing longer wavelengths than UVB, it can penetrate deeper into the skin and cause long-term damage with delayed manifestation. Irradiation of skin by UVA causes a cascade of cellular changes that can lead to skin cancer and premature ageing. Another UVA pathway to skin cancer is its effect on immunosuppression. A secondary effect of short-term tan by stimulating epidermal melanin is also associated with UVAs. Due to the consistency of its intensity, skin health professionals need to educate their patients on the daily application of broad-spectrum sunscreen all year round.
What are UVBs
UVB covers the wavelength of 280–320 nm and its intensity peaks at around midday. UVB is also the primary cause of burns. It delivers long-lasting tan and stimulates cells to produce thicker epidermis. Its effects are typically more acute and greater than UVA, such as erythema, stimulation of melanogenesis and in extreme cases, formation of blisters. Like UVA, DNA is also a chromophore for UVB, contributing to the risk of skin cancers. The beneficial effect of UVB is converting epidermal 7-dehydrocholesterol into vitamin D, hence short-term (10-15mins) of sun exposure before 10 am or after 3 pm is recommended.
What are UVCs
UVCs, the shortest wavelength of UV radiation (200–280 nm) and highly mutagenic, do not reach the Earth's surface because it is absorbed by stratospheric ozone.
Main effects of UV radiation on normal-appearing human skin
ACUTE (Cellular) | CLINICAL | CHRONIC |
|---|---|---|
DNA photodamage
Reactive oxygen species
Gene and protein expression
Apoptosis
Langerhans cell depletion
Vit D-photosynthesis
Nitrogen oxide relied (UVA) | Erythema
Skin tanning
Suppression of acquired immunity
Reduction of blood pressure via nitric oxide | Skin cancer
Photoageing epidermal |
UV-rays and skin response

Chen, H., Weng, Q. Y., & Fisher, D. E. (2014). UV signaling pathways within the skin. Journal of Investigative Dermatology, 134(8), 2080-2085. https://doi.org/10.1038/jid.2014.161
UV radiation activates the cutaneous immune system and this leads to an inflammatory skin response. Melanin in our skin tissue is the first line of defence mechanism against UV radiation. It absorbs UV radiation and converts it into heat. This melanin is further stimulated by the Melanocortin 1 Receptor, causing the manifestation of unwanted pigmentation and long-term tan. Keratinocytes undergo apoptosis due to UV-induced injury to avoid malignancy. UV exposure causes the synthesis of highly reactive oxygen species that place oxidative stress on the epidermal cells and cause DNA mutations. These mutations are the main pathway to epidermal malignancy and the development of skin cancers. Intermittent UVR exposure accumulates epidermal DNA damage, increasing the risk of melanoma. It is associated with 65% of melanoma cases and 90% of keratinocyte cancers.
Different skin types also respond differently to UV radiation. Fitzpatrick I-III have a higher susceptibility to the development of burns and skin cancer than Fitzpatrick IV-VI. This is due to the relative ease of UV penetration into the deeper layers of the epidermis and further damage to keratinocytes and melanocytes.
Consequences of UV Signalling Pathway Deficiency
Mutations to the tumour suppressor p53 are associated with human cancer as well as skin cancers. It regulates many signalling pathways that are activated in response to stimuli such as DNA damage, oxidative stress, and hypoxia and is responsible for DNA repair. Mutant p53 can be found in lesions of sun-exposed human skin.
UV Index
The UV Index is a tool created to communicate solar damage to the general public and help them decide the level of protection they need when leaving the house. UV Index measures the Minimal Erythemal Dose. This is the minimum required UV dose that can induce erythema and skin damage to the skin.
The UV Index is the measure of the level of UV radiation. This index varies throughout the day, with the highest level being at the solar noon (between noon and 2 pm)
(2023).How to prevent Melanoma[Image]. Melanoma Institute of Australia. https://melanoma.org.au/about-melanoma/how-to-prevent-melanoma/
The SunSmart app can be used to determine the UV Index throughout the day.
The UV Index divides UV radiation levels into:
low (1-2)
moderate (3-5)
high (6-7)
very high (8-10)
extreme (11 and above).
You can access the SunSmart app here
Myth busting – Skin Cancer
Below are some commonly held beliefs by the public about skin cancer. Skin health professionals play an important role in dispelling myths, and fears by conveying evidence-based information to support sun-safe behaviours.
Only fair-haired and light-skinned people get skin cancer
Skin cancer only happens when you are older
Skin cancer only happens in moles or freckles that have gone rogue
A tan (fake or real) will protect from burning and skin cancer
Melanotan is a safe way to tan
Only people who sunbathe or use solariums get skin cancer
You cannot get sunburned on cloudy or cold days
You can’t get sunburned behind glass (car or office window)
Facts about skin cancer risk
Both sexes experience skin cancer but men experience a higher risk due to environmental and behavioural influences.
Those that work or play for prolonged periods outdoors have a higher risk of skin cancer
More than five (5) blistering or peeling sunburns during childhood and teen years have been associated with an increased risk of skin cancer. This is important to educate on as even if someone stays out of the sun and uses sun-safe behaviours after the age of 30 their previous history can still impact on their risk.
Family history can increase your risk of skin cancer
Your Fitzpatrick phototype is associated with the risk of skin cancer (but it is prolonged sun exposure that causes skin cancer)
Increasing age is associated with a higher risk of skin cancer due to changes in the body's ability to detect and destroy damaged cells.
The number of freckles and moles, particularly atypical moles are associated with a higher risk of skin cancer.
Having received radiation therapy for cancer treatment or UV therapy for a skin condition may increase the risk of skin cancer
Recommendations & Sun Protective Behaviours
Disclaimer
The information in this document is general only and is not, and is not intended to be advice. Before making any decision or taking any action, you should consult with appropriate accounting, tax, legal or other advisors. No warranty is given as to the correctness of the information contained in this publication, or of its suitability for use by you. To the fullest extent permitted by law, the Australian Society of Dermal Clinicians Inc. (ASDC) is not liable for any statement or opinion, or for any error or omission contained in this publication and disclaims all warranties with regard to the information contained in it, including, without limitation, all implied warranties of merchantability and fitness for a particular purpose. ASDC is not liable for any direct, indirect, special, or consequential losses or damages of any kind, or loss of profit, loss or corruption of data, business interruption, or indirect costs, arising out of or in connection with the use of this publication or the information contained in it, whether such loss or damage arises in contract, negligence, tort, under statute, or otherwise
REFERENCE LIST:
Amaris N. Geisler, Evan Austin, Julie Nguyen, Iltefat Hamzavi, Jared Jagdeo, Henry W. Lim, Visible light. Part II: Photoprotection against visible and ultraviolet light, Journal of the American Academy of Dermatology, Volume 84, Issue 5, 2021, Pages 1233-1244, ISSN 0190-9622, https://doi.org/10.1016/j.jaad.2020.11.074.
Ansary TM, Hossain MR, Kamiya K, Komine M, Ohtsuki M. Inflammatory Molecules Associated with Ultraviolet Radiation-Mediated Skin Aging. International Journal of Molecular Sciences. 2021; 22(8):3974. https://doi.org/10.3390/ijms22083974
Cancer Council. (n.d.). UV Index. https://www.cancer.org.au/cancer-information/causes-and-prevention/sun-safety/uv-index
Chen, H., Weng, Q. Y., & Fisher, D. E. (2014). UV signalling pathways within the skin. Journal of Investigative Dermatology, 134(8), 2080-2085. https://doi.org/10.1038/jid.2014.161
Heckman CJ, Liang K, Riley M. Awareness, understanding, use, and impact of the UV index: A systematic review of over two decades of international research. (2019) 123:71-83. doi: 10.1016/j.ypmed.2019.03.004.
Lee, J.W., Ratnakumar, K., Hung, K.-F., Rokunohe, D. and Kawasumi, M. (2020), Deciphering UV-induced DNA Damage Responses to Prevent and Treat Skin Cancer. Photochem Photobiol, 96: 478-499. https://doi.org/10.1111/php.13245
Mohania, D., Chandel, S., Kumar, P., Verma, V., Digvijay, K., Tripathi, D., ... & Shah, D. (2017). Ultraviolet radiations: Skin defense-damage mechanism. Ultraviolet Light in Human Health, Diseases and Environment, 71-87.
Moshammer, H., Simic, S., & Haluza, D. (2016). UV “Indices”—What do they indicate?. International Journal of Environmental Research and Public Health, 13(10), 1041. https://doi.org/10.3390/ijerph13101041
O'Connor C, Rafferty S, Murphy M. A qualitative review of misinformation and conspiracy theories in skin cancer. Clin Exp Dermatol. 2022 Oct;47(10):1848-1852. doi: 10.1111/ced.15249. Epub 2022 Jun 15. PMID: 35514125; PMCID: PMC9796846.
Piipponen M, Riihilä P, Nissinen L, Kähäri V-M. (2021)The Role of p53 in Progression of Cutaneous Squamous Cell Carcinoma. Cancers. 13(18):4507. https://doi.org/10.3390/cancers13184507
Sander M, Sander M, Burbidge T, Beecker J. The efficacy and safety of sunscreen use for the prevention of skin cancer. CMAJ. 2020 Dec 14;192(50):E1802-E1808. doi: 10.1503/cmaj.201085. PMID: 33318091; PMCID: PMC7759112.
The WHO. (2022). Radiation: The ultraviolet (UV) index. https://www.who.int/news-room/questions-and-answers/item/radiation-the-ultraviolet-(uv)-index
Yao Ke, Xiao-Jing Wang (2021).TGFβ Signaling in Photoaging and UV-Induced Skin Cancer, Journal of Investigative Dermatology, 141(4) Supplement 1104-1110, https://doi.org/10.1016/j.jid.2020.11.007.

















Comments